Mechanisms of Disease in Preterm Labor and Complications of Prematurity; Prenatal Diagnosis of Congenital Anomalies
- Roberto Romero,
MD, DMedSci, Chief, Pregnancy Research Branch

Preterm birth is the leading cause of perinatal morbidity and mortality worldwide, and two-thirds of all preterm births occur after the onset of preterm labor. The cost of prematurity in the United States alone was estimated at $26 billion per year in 2007. Therefore, important goals are to understand the mechanisms of disease responsible for preterm birth and fetal injury and to improve the prediction and prevention of preterm birth. The Pregnancy Research Branch (PRB) proposed that preterm parturition is a syndrome caused by multiple pathologic processes [Romero R et al. Science 2014;345:760]. The Branch developed methods for the rapid diagnosis of intra-amniotic infection/inflammation and showed that such pathologic processes can be treated successfully. In addition, the current approach to predict and prevent spontaneous preterm birth in clinical obstetrics is based on the work of the Branch (the PREGNANT trial and subsequent meta-analyses). The research team continues to study the physiology of pregnancy and parturition to inform studies of spontaneous preterm labor, and, in particular, the use of high-dimensional, post-genomic tools, such as transcriptomics, proteomics, and the analysis of parturition at single-cell resolution.
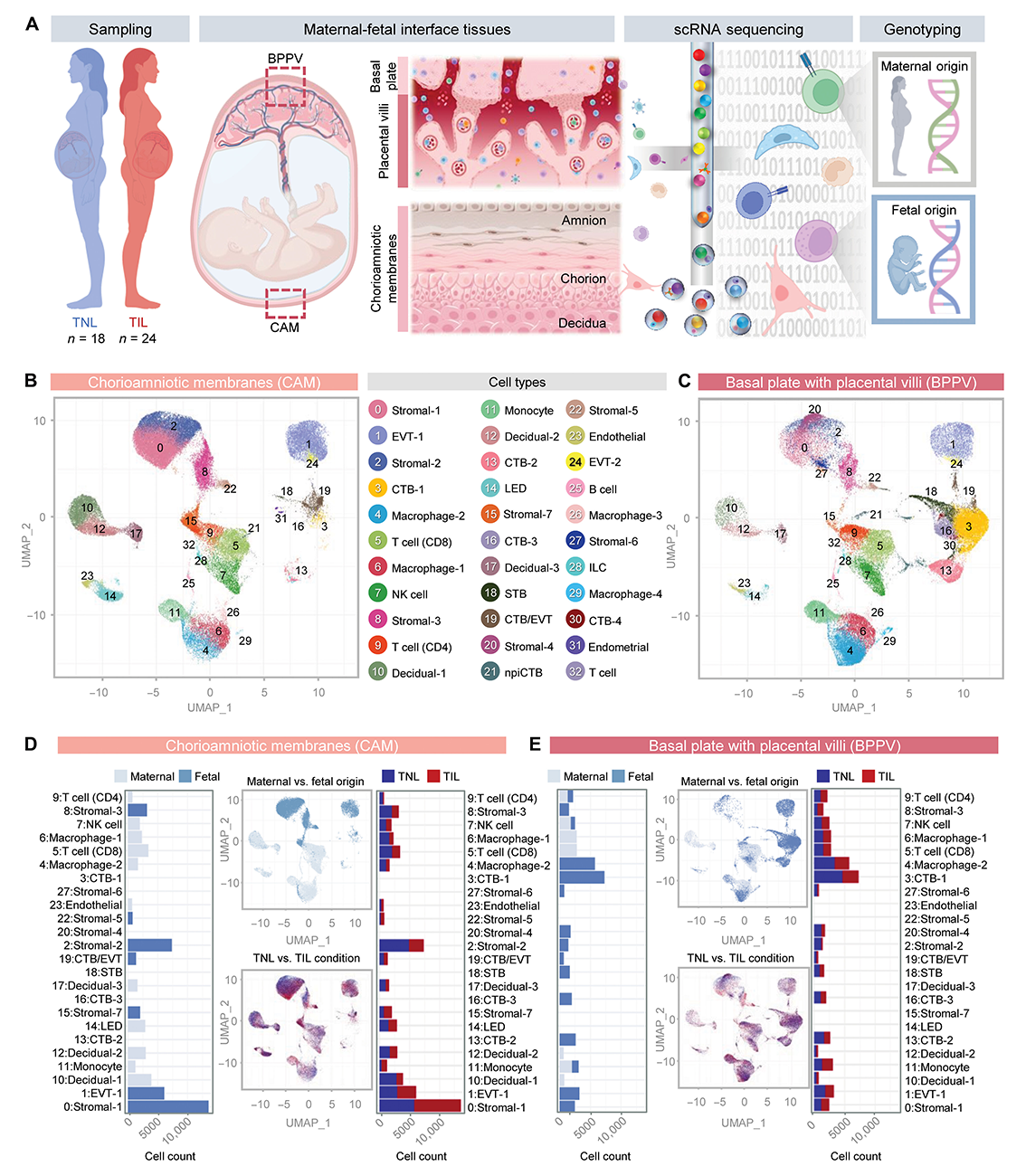
Figure 1. Single-cell atlas of the maternal-fetal interface in parturition
A. Study design showing the collection of placental tissues from women who delivered at term with (TIL, n = 24) or without (TNL, n = 18) labor. Briefly, CAMs (chorioamniotic membranes) and the BPPV (basal plate with placental villi) were sampled to generate single-cell suspensions for scRNA-seq. Genotyping of maternal and neonatal tissues was also performed to allow assignment of maternal (M) or fetal (F) origin to cells.
B. and C. Uniform manifold approximation and projection (UMAP) plots show all cell types identified in the (B) CAM and (C) BPPV.
D. and E. Bar plots represent the total numbers of each maternal (light blue) or fetal (dark blue) cell type in the (D) CAM and (E) BPPV, and the numbers of each cell type with labor (red bars) and without labor (blue bars). Corresponding UMAP plots show the cell clusters in the CAM and BPPV according to maternal (light blue) or fetal (dark blue) origin and how each changes with labor (red clusters) and without labor (blue clusters).
Figure 1. Single-cell atlas of the maternal-fetal interface in parturition
A. Study design showing the collection of placental tissues from women who delivered at term with (TIL, n = 24) or without (TNL, n = 18) labor. Briefly, CAMs (chorioamniotic membranes) and the BPPV (basal plate with placental villi) were sampled to generate single-cell suspensions for scRNA-seq. Genotyping of maternal and neonatal tissues was also performed to allow assignment of maternal (M) or fetal (F) origin to cells.
B. and C. Uniform manifold approximation and projection (UMAP) plots show all cell types identified in the (B) CAM and (C) BPPV.
D. and E. Bar plots represent the total numbers of each maternal (light blue) or fetal (dark blue) cell type in the (D) CAM and (E) BPPV, and the numbers of each cell type with labor (red bars) and without labor (blue bars). Corresponding UMAP plots show the cell clusters in the CAM and BPPV according to maternal (light blue) or fetal (dark blue) origin and how each changes with labor (red clusters) and without labor (blue clusters).
Imaging is a powerful instrument for scientific discovery and has changed the practice of obstetrics and maternal-fetal medicine. The single most important step that has made fetal medicine a discipline is the transformation of the fetus from an invisible to a visible subject through the use of imaging techniques, in particular, ultrasound. The technology has allowed the definition of fetal anatomy, biometry, and growth as well as the study of physiologic parameters, e.g., cardiac function, fetal sleep, and breathing. We use different imaging modalities to examine the diagnosis of anomalies and obstetrical syndromes. Such modalities include ultrasound (2-dimensional, 3-dimensional), magnetic resonance imaging, and optical methods. We have also utilized other imaging techniques to study the human placenta.
Sterile intra-amniotic inflammation can be successfully treated by blocking Interleukin-6: a novel approach to reduce preterm labor and neonatal morbidity and mortality
Intra-amniotic inflammation is a major cause of the preterm labor syndrome and can be the result of microbial-induced inflammation (intra-amniotic infection) or sterile inflammation. We identified alarmins (host products released during cellular stress or necrosis as a cause of alarmin-induced premature labor). There is a need to develop new treatment modalities for sterile intra-amniotic inflammation. Previous work at the Perinatology/Pregnancy Research Branch indicated that interleukin-6 (IL-6) and interleukin-1α (IL-1α), an alarmin, were involved in sterile-induced intra-amniotic inflammation in patients with premature labor. Therefore, we reason that the blockade of IL-6 may prevent preterm birth and neonatal morbidity. To test this hypothesis, we developed a murine model of sterile-induced inflammation preterm birth using ultrasound-guided intra-amniotic injection of IL-1α. We tested whether the blockade of IL-6 using an antibody against the IL-6 receptor (anti-IL-6R or aIL-6R) could prevent preterm birth and adverse neonatal outcomes. Targeted transcriptomic profiling assessed maternal, fetal, and neonatal inflammation. Neurodevelopment was assessed after birth.
Intra-amniotic injection of IL-1α induced sterile intra-amniotic inflammation, including preterm labor and delivery and neonatal mortality. Prenatal treatment with aIL-6R significantly reduced the frequency of IL-1α–induced preterm birth (50% vs. 7%) by dampening inflammatory processes associated with the common pathway of labor. Importantly, aIL-6R also significantly reduced neonatal mortality (56% vs. 22%). aIL-6R crossed from the maternal circulation to the amniotic cavity and dampened the fetal organ inflammation, which was associated with improved fetal growth. The beneficial effects of prenatal IL-6R blockade extended to neonatal life, as there was evidence of improved survival, growth, neurodevelopment, and gut immune homeostasis. Collectively, this work provides an approach for the treatment of intra-amniotic sterile inflammation, which is the most common form of inflammation in patients with premature labor and intact membranes and in those with cervical insufficiency.
Deciphering maternal-fetal cross-talk in the human placenta during parturition using single-cell RNA sequencing
There are 140 million deliveries per year, and most occur through the process of labor. Parturition is a complex physiological process involving a well orchestrated dialogue between the mother and fetus. However, the cellular contributions and communications that facilitate maternal-fetal cross-talk in labor have not been elucidated. To understand this process, we have used single-cell RNA sequencing (scRNA-seq) to decipher maternal-fetal signaling in the human placenta during term and preterm labor.
We first generated a single-cell atlas of different sites of the human placenta (chorioamniotic membranes and basal plate) in patients in labor and those not in labor at term. We found that maternal and fetal cell types undergo changes in transcriptomic activity during labor. The cell types most affected by labor were fetal stromal and maternal decidual cells in the chorioamniotic membranes and maternal and fetal myeloid cells in the basal plate. Cell-cell interaction analyses showed that chorioamniotic membranes and basal-plate cell types participated in labor-driven maternal and fetal signaling, including the collagen, C-X-C motif ligand (CXCL), tumor necrosis factor (TNF), galectin, and IL-6 pathways.
We then explored whether scRNA-seq data of the placenta could be integrated with publicly available bulk transcriptomic data from the maternal circulation. We showed that: (1) placenta-derived scRNA-seq signatures could be monitored in the maternal circulation throughout gestation and in labor; (2) by comparative analysis, placenta-derived signatures in term labor were mirrored by those in spontaneous preterm labor and birth; and 3) that placenta-derived signatures could be detected in the maternal circulation in patients who subsequently developed spontaneous preterm labor with either intact or ruptured membranes.
Our findings provide insight into the maternal-fetal dialogue at the time of human parturition at term. Importantly, we found that the placenta-derived single-cell signatures of parturition at term can be identified at the time of diagnosis of preterm labor and weeks before preterm labor and delivery. This therefore suggests that analysis of the maternal circulation allows non-invasive prediction of spontaneous preterm birth, the major challenge to obstetrics in the 21st century. We were successful at reducing the rate of preterm birth by identifying biomarkers in the mid-trimester (a sonographic short cervix) and timely intervention (vaginal progesterone). The work with scRNA-seq of the human placenta and circulating analysis of nucleic acids holds promise for the prediction and prevention of spontaneous preterm birth.
Preeclampsia at term: evidence of differential engagement of the angiogenic/antiangiogenic systems and intravascular inflammation
Preeclampsia/eclampsia is a serious complication of pregnancy, which increases maternal and neonatal morbidity and mortality. The condition is syndromic, given its multiple etiologies. Two important mechanisms of disease implicated in the pathophysiology of preeclampsia are: (1) intravascular inflammation; and (2) antiangiogenic state. On the basis of the profiles of angiogenic/antiangiogenic factors in the maternal circulation, patients with preeclampsia at term may be classified into two subgroups, with different clinical characteristics and prevalence of adverse outcomes. To understand whether patients with an abnormal angiogenic profile also have evidence of exaggerated inflammation as do patients diagnosed with preeclampsia at term, we studied patients with preeclampsia at term, which contributed the most to maternal death as a result of this syndrome. Therefore, we studied the plasma profiles of cytokines and chemokines in patients with preeclampsia at term as a function of a normal or abnormal antiangiogenic profile. We conducted a nested case-control study to include patients classified into three groups: patients with an uncomplicated pregnancy and patients with preeclampsia at term with a normal or an abnormal angiogenic profile.
We found that patients with preeclampsia at term and an abnormal angiogenic profile showed evidence of the greatest degree of intravascular inflammation among the study groups. These patients had higher plasma concentrations of four cytokines (IL-6, IL-12/IL-23p40, IL-15, and IL-16) and eight chemokines (IL-8, eotaxin, eotaxin-3, interferon-γ inducible protein-10, monocyte chemotactic protein-4, macrophage inflammatory protein-1β, macrophage-derived chemokine, and thymus and activation-regulated chemokine) compared with patients with an uncomplicated pregnancy. By contrast, patients with preeclampsia at term and a normal angiogenic profile, compared with patients with an uncomplicated pregnancy, had only a higher plasma concentration of monocyte chemotactic protein-4. Our observations suggest that preeclampsia at term can be classified into two clusters: one is characterized by an antiangiogenic state coupled with an excessive inflammatory process, whereas the other has neither of these features. Collectively, these observations reaffirm the syndromic nature of the condition and open avenues for the prediction, classification, and prevention of preeclampsia at term.
New labor curves of dilation and station to improve the accuracy of predicting labor progress
Of the 140 million births per year, 21% occur through cesarean delivery. Failure to progress in labor is the most common indication for intrapartum cesarean delivery, and its diagnosis is based on the assessment of cervical dilation and station over time. Labor curves serve as references for expected changes in dilation and fetal descent. The labor curves of Friedman and subsequent formulations of this are based on time alone and derived from mothers with spontaneous labor onset. However, labor induction is now common, and clinicians also consider other factors when assessing labor progress (e.g., contraction frequency, rupture of membranes, etc.). Labor curves that consider the use of labor induction and other factors that influence labor progress have the potential to be more accurate and closer to clinical decision-making.
Our study aimed to compare the prediction errors of labor curves based on a single factor (time) or multiple clinically relevant factors using two modeling methods: mixed-effects regression, a standard statistical method, and Gaussian processes, a machine learning method.
This was a longitudinal cohort study of changes in dilation and station based on data from 8,022 births in nulliparous women with a live, singleton, vertex-presenting fetus at or over 35 weeks of gestation with a vaginal delivery. New labor curves of dilation and station were generated with 10-fold cross-validation. External validation was performed using a geographically independent group. Model variables included: time from the first examination in the 20 hours before delivery; dilation, effacement, and station recorded at the previous examination; cumulative contraction counts; and use of epidural anesthesia and labor induction. To assess model accuracy, differences between each model's predicted value and its corresponding observed value were calculated. These prediction errors were summarized using mean absolute error and root mean squared error statistics.
We found that dilation curves based on multiple parameters were more accurate than those derived from time alone. The mean absolute error of the multifactor methods was significantly better (lower) than those of the single-factor methods. The root mean squared errors of the multifactor methods were also significantly better (lower) than those of the single-factor methods. The multifactor machine-learning dilation models showed small but statistically significant improvements in accuracy over the mixed-effects regression models. The multifactor machine learning method produced a curve of descent with a mean absolute error of 0.512 cm and a root mean squared error of 0.660 cm. External validation using independent data produced similar findings.
We conclude that cervical dilation models based on multiple clinically relevant parameters showed improved (lower) prediction errors than models based on time alone. The mean prediction errors were reduced by more than 50%. A more accurate assessment of departure from expected dilation and station may help clinicians optimize intrapartum management.
Maternal physical activity in early pregnancy alters the size of the yolk sac and embryonic dimensions, and is modulated by embryonic sex.
The relationship between maternal physical activity, early fetal growth, and yolk-sac dimensions is unknown. We performed a longitudinal study to characterize the relationship between maternal physical activity measured through actigraphy, and yolk-sac size and embryonic dimensions. The yolk sac, a transient extra-embryonic organ, plays a crucial role in embryonic development and is involved in metabolism, nutrition, growth, and hematopoiesis. Prospectively collected data from 190 healthy women indicated that their total daily physical activity, including both light and moderately vigorous activity, was significantly associated with yolk-sac growth dynamics depending on embryonic sex and gestational age. Higher preconception maternal physical activity was significantly linked to a larger yolk sac at 7 weeks and a smaller yolk sac at 10 weeks gestation in male embryos; in female embryos, the yolk-sac size was increased at 10 weeks gestation and was, on average, 24% larger than that in male embryos. Considering the pattern of other maternal effects on yolk-sac size, e.g., body composition and sleep duration, we suggest that physiological yolk-sac adaptations occur in short, sex-specific time windows and can be influenced by maternal factors.
Publications
- Blockade of IL-6R prevents preterm birth and adverse neonatal outcomes. EBioMedicine 2023 98:104865
- Deciphering maternal-fetal cross-talk in the human placenta during parturition using single-cell RNA sequencing. Sci Transl Med 2024 16(729):eadh8335
- Preeclampsia at term: evidence of disease heterogeneity based on the profile of circulating cytokines and angiogenic factors. Am J Obstet Gynecol 2024 450.e1–450.e18
- New labor curves of dilation and station to improve the accuracy of predicting labor progress. Am J Obstet Gynecol 2024 231(1):1–18
- Maternal physical activity affects yolk sac size and growth in early pregnancy, but girls and boys use different strategies. Sci Rep 2023 13(1):20246
Collaborators
- Piya Chaemsaithong, MD, PhD, Mahidol University, Bangkok, Thailand
- Tinnakorn Chaiworapongsa, MD, Wayne State University School of Medicine, Detroit, MI
- Agustin Conde-Agudelo, MD, Wayne State University School of Medicine, Detroit, MI
- Amir Gandjbakhche, PhD, Section on Translational Biophotonics, NICHD, Bethesda, MD
- Nardhy Gomez-Lopez, PhD, Washington University School of Medicine, St. Louis, MO
- Adi L. Tarca, PhD, Wayne State University, Detroit Medical Center, Detroit, MI
- Bo Hyun Yoon, MD, PhD, Seoul National University, Seoul, Korea
Contact
For more information, email romeror@mail.nih.gov or visit https://irp.nih.gov/pi/roberto-romero.