You are here: Home > Section on Growth and Obesity
Physiology, Psychology, and Genetics of Obesity

- Jack A. Yanovski, MD, PhD, Head, Section on Growth and Obesity
- Joan C. Han, MD, Assistant Clinical Investigator
- Asem Ali MD, Clinical Fellow, Endocrine Training Program
- Melissa K. Crocker, MBA, MD, Clinical Fellow, Endocrine Training Program
- Lauren B. Shomaker, PhD, Special Volunteer
- Roya Sherafat, MD, PhD, Special Volunteer
- Diane C. Adler-Wailes, MS, Biologist
- Sheila M. Brady, RN, FNP, Nurse Practitioner
- Shannon Fuhr, BA, Postbaccalaureate Fellow
- Caroline A. Roza, BS, Postbaccalaureate Fellow
- Yasmmyn Salinas, BS, Postbaccalaureate Fellow
- Mahsa Sorouri, BS, Postbaccalaureate Fellow
- Babette Stern, BS, Postbaccalaureate Fellow
- Jaclyn Zocca, BA, Postbaccalaureate Fellow
The prevalence of overweight and obesity in children and adults has tripled during the past 40 years. The alarming rise in body weight has likely occurred because the current environment affords easy access to calorie-dense foods and requires less voluntary energy expenditure. However, this environment leads to obesity only in those individuals whose body weight–regulatory systems are not able to control body adiposity with sufficient precision in our high calorie/low activity environment, which suggests there are subgroups in the US with a uniquely high susceptibility to weight gain under the prevailing environmental conditions. The primary goal of the Section on Growth and Obesity is to elucidate the genetic underpinnings of the metabolic and behavioral endophenotypes that contribute to the development of obesity in children. Using our unique longitudinal cohort of children at risk for adult obesity who have undergone intensive metabolic and behavioral phenotyping, we examine genetic and phenotypic factors predictive of progression to adult obesity in children who are in the "pre-obese" state, allowing characterization of phenotypes unconfounded by the impact of obesity itself. Once identified as linked to obesity, genetic variants that impair gene function are studied intensively. These approaches are expected to improve our ability to predict which children are at greatest risk for obesity and its comorbid conditions and to lead to more targeted, etiology-based prevention and treatment strategies for pediatric obesity.
Molecular studies of factors important for childhood body weight regulation
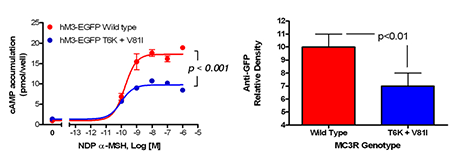
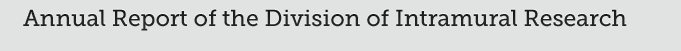
Figure 1.
Studies of a human MC3R variant containing two naturally occurring polymorphisms—a variant that was associated with pediatric-onset obesity—found that the variant was partially inactive, with decreased signal transduction (left panel), likely due to reduced protein expression (right panel). (click image to enlarge)
To identify gene variants impacting body composition, we have been examining polymorphisms in genes involved in the leptin signaling pathway. Such genes include proopiomelanocortin (POMC), the melanocortin 3 receptor (MC3R), brain-derived neurotrophic factor (BDNF) FTO, and histaminergic receptors 1 and 3. We are currently studying a variant MC3R that is associated with adiposity in children and that appears to have functional significance for MC3R signal transduction. Children who were homozygous variant for both the polymorphisms Thr6Lys and Val81Ile had significantly greater BMI-SD score, fat mass, body circumference measurements, and higher plasma levels of insulin and leptin compared with "wild-type" or heterozygous children. In vitro studies subsequently found that signal transduction and protein expression were significantly lower for the double mutant MC3R (Figure 1). Ongoing studies attempt to understand the mechanisms by which these sequence alterations impact body weight. We found that children homozygous variant for both the polymorphisms Thr6Lys and Val81Ile showed no deficits in energy expenditure but demonstrated hyperphagia in laboratory meal studies (Figure 2). The results were specific to function-altering mutations and not associated with other common polymorphisms that we identified in the MC3R. In collaboration with Heiner Westphal, we developed transgenic "knock-in" mice expressing the human wild-type and human double-mutant MC3R; the mice will be studied during the next two years.
Figure 2.
Energy intake is studied using free access buffet meals of palatable foods. Children homozygous for two polymorphisms in the MC3R consumed more at the buffet than heterozygotes or those who had wild-type MC3R. (click image to enlarge)
We also recently investigated the BDNF-TrkB pathway as it relates to body mass in children. We measured serum BDNF in a group of 328 children, age 3-19, a high proportion of whom were extremely obesity. BDNF was significantly lower in obese children (p=0.03); in multiple regression analyses with log-BDNF as the dependent variable, BMI (p=0.03), BMI-Z (p=0.01), and body fat (p's<0.02), were all negatively associated with BDNF. These data suggested that some obese individuals with low serum BDNF for age may have mutations that alter BDNF function. Another initiative assessed the role of BDNF haploinsufficiency as a cause of obesity in patients with syndromes that are attributable to deletions in the vicinity of 11p14.1, where the human BDNF gene is found. Using a comparative genomic hybridization approach that is verified with PCR-based assays, we are examining genotype-phenotype relationships in patients with 11p deletion syndromes such as the WAGR (Wilms Tumor, Aniridia, Genitourinary, and Renal abnormalities) syndrome. In 33 subjects with heterozygous 11p deletions ranging in size from 1.0-26.5 Mb, 19 had regions of deletion that involved the BDNF gene (BDNF+/−). BDNF+/− individuals had significantly greater body mass during childhood, starting at age 2y (Figure 3) than those with intact BDNF (BDNF+/+). All (95% CI: 76.8-100%) BDNF+/− individuals were obese by age 10 while only 20% (95%CI: 2.5-55.6%) of BDNF+/+ (P<0.0001) were. Analysis of the telomeric deletion boundaries of patients indicated the presence, within 80 kb of the BDNF exon, of a critical region for pediatric-onset obesity (Figure 3). One obese subject exhibited deletion of BDNF exons I-III but preservation of subsequent BDNF exons. Each subject who maintained normal weight during childhood had a deletion that did not involve BDNF. Our findings suggest that BDNF haploinsufficiency in patients with WAGR syndrome leads to pediatric-onset obesity. A clinical protocol admitting patients with WAGR syndrome and other 11p deletion syndromes for a full characterization of their energy intake and expenditure is now ongoing. A second research direction involves characterizing the body composition and energy homeostasis of mice with selective replacement of several of the BDNF promoter regions that create unique BDNF splice variants with GFP. We hypothesize that mice lacking splice variants created by early promoter regions (I through III) will show obesity, while later promoters will be of less importance for hypothalamic BDNF function.
Physiology, metabolism, and psychology of childhood body weight regulation

Figure 3.
Patients with WAGR Syndrome who have haploinsufficiency for brain-derived neurotrophic factor (BDNF) had higher BMI standard deviation score (BMI Z-Score) than children and adults with WAGR Syndrome who retained two copies of BDNF. Deletions that extended into exon 1 of BDNF were associated with 100% risk of childhood-onset obesity. (click image to enlarge)
Our studies are directed at understanding the physiological, psychological, and metabolic factors that place children at risk for undue weight gain. As part of these studies, we examined how best to measure eating-related psychopathology, insulin sensitivity, changes in body composition, energy intake, and energy expenditure in children and we studied the short- and long-term stability of the components of metabolic syndrome. We found that leptin is an important predictor of weight gain in children: when followed longitudinally, we found that those with high leptin gain even more weight than those with lower leptin levels. Additional studies that are anticipated to begin in the next year will test specific therapies directed at ameliorating inadequate leptin signaling specifically in conditions that are marked by leptin receptor hypofunction.
Recent investigations have also documented how hyperinsulinemia is related to energy intake in non-diabetic, obese children who selected lunch from a 9,835kcal buffet (Figure 2) eaten ad libitum after an overnight fast. Energy intake was positively associated with the fasting homeostasis model assessment for insulin resistance index (HOMA-IR; beta = 0.24, p=0.042), fasting insulin/glucose ratio (beta = 0.24, p=0.044), first-phase insulin (beta = 0.23, p=0.032), and first-phase C-peptide (beta = 0.21, p=0.046) during a hyperglycemic clamp; energy intake was negatively associated with clamp-derived insulin sensitivity (SIclamp; beta = -0.29, p=0.042). Each 10% decrease in SIclamp predicted 27 kcal greater energy intake. These associations suggest mechanisms whereby insulin resistance may contribute to excessive weight gain in children and have informed some of our treatment approaches to pediatric obesity (described below).
Our evaluations of binge-eating behaviors in children suggest that such behaviors also are associated with adiposity in children. We also found that binge eating and dieting behaviors may predict future weight gain in children at risk for obesity; children reporting binge-eating behaviors such as loss of control over eating gained, on average, a mean of 2.4 kg more per year than non-binge-eating children (see reference 3). Our data also suggest that children endorsing binge eating consume more energy during meals. Actual intake during buffet meals averaged 400 kcal more in children with binge eating; however, despite their greater intake, such children reported shorter-lived satiety than children who did not engage in binge-eating episodes. The ability to consume large quantities of palatable foods, especially when coupled with decreased subsequent satiety, may play a role in the greater weight gain found in binge-eating children. These data also suggest that interventions targeting disordered eating behaviors may be useful in preventing excessive fat gain in children prone to obesity. Because binge eating appears to be an African American heritable trait, we have also initiated studies to investigate potential genetic factors linked to loss of control over eating (see reference 4). We genotyped 229 youth aged 6-19 y for FTO SNP rs9939609, conducted body-composition measurements, and interviewed them to determine the presence or absence of loss-of-control (LOC) eating. Subjects with at least one A allele (67.7%) had significantly greater BMI, BMI z scores (P < 0.01), and fat mass (P < 0.05). Of the AA/AT subjects, 34.7% reported LOC compared with 18.2% of the TT (homozygous for wild-type alleles) subjects (P = 0.002). AA/AT subjects consumed a greater percentage of energy from fat than did the TT subjects (P < 0.01).
In order to determine the factors that are most important for developing the complications of obesity in youth, we study normal-weight children and adolescents, children who are already obese, and the non-obese children of obese parents, in two ongoing protocols. We examine body composition, metabolic rate, insulin sensitivity, glucose disposal, energy intake at buffet meals, and genetic factors believed to regulate metabolic rate and body composition. Psychological and behavioral factors, such as propensity to engage in binge-eating behavior, are also studied. We are studying children longitudinally into adulthood. In two protocols, we study food consumption of children during meals, to elucidate differences in the calorie and macronutrient content of meals and the circulating hormones related to hunger and satiety in those who either endorse binge-eating behaviors or report no such behaviors. We hypothesize that differences in these factors will predict the development of obesity in the populations studied and that they may be of great importance in developing rational approaches for the prevention and treatment of obesity in the diverse US population. A new clinical protocol based on a successful pilot study is examining the effects of a targeted interpersonal therapy intervention on body weight change in adolescents who endorse binge-eating behaviors.
Treatment of obesity and the co-morbid conditions associated with obesity
Given the rapid increase in the prevalence of obesity, the development of treatments for obesity in children and adults is urgently needed. In four clinical protocols, we examined approaches for the prevention and treatment of excessive body weight. We completed a pilot study demonstrating that severely obese adolescents can lose weight when enrolled in a comprehensive weight management program that includes the gastrointestinal lipase inhibitor orlistat as an adjunct to a behavioral modification program.
We recently completed a placebo-controlled randomized trial studying whether the weight loss of African American and Caucasian children and adolescents who have obesity-related comorbidities was enhanced by the use of orlistat 120 mg TID. Subjects participated in a 12-week weight reduction program. Body weight and body composition (by DXA and air displacement plethysmography), glucose homeostasis by the frequently sampled intravenous glucose tolerance test (FSIGT), fasting lipids, pulse, and blood pressure were compared before and after treatment. We studied 200 adolescents, 65% female, 61% African American, mean age ±SEM 14.6±0.10y, BMI 41.7±0.6 kg/m2 (range 27-87 kg/m2), with 85.5% of subjects completing the trial. Adolescents treated with orlistat lost more weight (P=0.011), BMI units (P=0.002), and fat mass (P=0.029). Although pulse and blood pressure decreased during the trial (P<0.001), orlistat treatment did not significantly alter these variables (all P>0.25). Similarly, HOMA-IR, SI by FSIGT, Apo B, total and LDL-cholesterol, and triglycerides decreased in proportion to weight loss (P<0.001), but orlistat use was not associated with significant reductions in any of these obesity-related laboratory comorbidities (all P>0.2). Both AST (+1.8±0.9 vs. -1.08±0.9, P=0.024) and ALT (+1.3±1.1 vs. -2.4±1.2, P=0.022) unexpectedly increased significantly with orlistat treatment. We concluded that orlistat added to a behavioral program significantly improved weight loss over a 6-month interval, but had little impact on obesity-related co-morbid conditions in obese adolescents.
A second, now completed study examined the mechanism by which metformin may affect the body weight of younger children who have hyperinsulinemia and are therefore at risk for later development of type 2 diabetes. We conducted a single-center, 6-month, randomized, double-blind, placebo-controlled trial of the effects of metformin, 1000 mg BID administered with meals, in severely obese children (6-12y) who manifested hyperinsulinemia and insulin resistance. Subjects participated in a monthly dietitian-administered weight reduction program. Body mass index and body composition (by air displacement plethysmography), glucose homeostasis (by HOMA-IR), and lipids were measured before and after 6-months' treatment. Between October 2000 and April, 2007, we enrolled 100 obese children (60% female, 11% Hispanic, 3% Asian, 40% African American), mean age 10.2±1.5y, with mean BMI 34.6±6.6 kg/m2 (range 23-58 kg/m2), with 85% of subjects (84% given metformin and 86% given placebo) completing the trial. In those randomized to metformin, BMI (P=0.006), BMI-Z score (P=0.02), and body fat mass (P<0.001) declined to a significantly greater extent than in placebo-treated children. Serum glucose (P=0.018) and HOMA-IR (P=0.05) also declined more in metformin-treated than in placebo-treated children. We concluded that metformin, added to a monthly behavioral program, significantly improved weight loss and reduced insulin resistance over a 6-month interval in severely obese, insulin-resistant children.
A third clinical trial in adults examined the role dietary calcium plays in body weight (see reference 5). We randomized 340 overweight (BMI 25 to <30 kg/m2) and obese (BMI ≥30 kg/m2) adults to take calcium carbonate (elemental calcium, 1500 mg/d, n = 170) or placebo (n = 170) with meals for 2 years, with 75% of participants completing the trial (78% received calcium; 73% received placebo). There were no statistically or clinically significant differences between the calcium and placebo groups in change in body weight (difference, 0.02 kg, 95% CI, −1.64 to 1.69 kg; P = 0.98), BMI (difference, 0.32 kg/m2, CI, −0.41 to 1.02 kg/m2; P = 0.39), or body fat mass (difference, 0.39 kg, CI, −1.04 to 1.92 kg; P = 0.55). Parathyroid hormone concentrations declined more in the calcium group than in the placebo group (difference, −0.71 pmol/L, CI, −1.28 to −0.13 pmol/L). We concluded that dietary supplementation with elemental calcium, 1500 mg/d, for two years had no statistically or clinically significant effects on weight in overweight and obese adults. Calcium supplementation is unlikely to have clinically significant efficacy in preventing weight gain in such patients.
A fourth, recently completed study examined the role that central nervous system histamine plays in controlling food intake at meals.
Additional Funding
- NIH Clinical Center "Bench to Bedside" Award: FTO and Eating in Absence of Hunger 2009-2011
- NIH Clinical Center "Bench to Bedside" Award: Histaminergic Pathways and Energy Intake in Obese Women 2008-2010
- Prader-Willi Syndrome Association (USA) Best Idea Grant for Hyperphagia Research
Publications
- Savastano DM, Tanofsky-Kraff M, Han JC, Ning C, Sorg RA, Roza CA, Wolkoff LE, Jefferson-George KS, Figueroa RE, Sanford EL, Brady S, Kozlosky MS, Schoeller DA, Yanovski JA. Energy intake and energy expenditure among children with polymorphisms of the melanocortin-3 receptor. Am J Clin Nutr 2009;90:912-920.
- Han JC, Liu QR, Jones M, Levinn RL, Menzie CM, Jefferson-George KS, Adler-Wailes DC, Sanford EL, Lacbawan FL, Uhl GR, Rennert OM, Yanovski JA. Brain derived neurotrophic factor and obesity in WAGR syndrome. New Engl J Med 2008;359:918-927.
- Tanofsky-Kraff M, Yanovski SZ, Schvey NA, Olsen CH, Gustafson J, Yanovski JA. A prospective study of loss of control eating for body weight gain in children at high risk for adult obesity. Int J Eat Disord 2009;42:26-30.
- Tanofsky-Kraff M, Han JC, Anandalingam K, Shomaker LB, Columbo KM, Wolkoff LE, Kozlosky M, Elliott C, Ranzenhofer LM, Roza CA, Yanovski SZ, Yanovski JA. The FTO gene rs9939609 obesity-risk allele and loss of control over eating. Am J Clin Nutr 2009;90:1483-8.
- Yanovski JA, Parikh SJ, Yanoff LB, Denkinger BI, Calis KA, Reynolds JC, Sebring NG, McHugh T. Effects of calcium supplementation on body weight and adiposity in overweight and obese adults: a randomized trial. Ann Intern Med 2009;150:821-829.
Collaborators
- Greti Aguilera, MD, Program on Developmental Endocrinology and Genetics, NICHD, Bethesda, MD
- Leslie Biesecker, MD, GDRB/HDS, NHGRI, Bethesda, MD
- Kong Chen, PhD, Clinical Endocrinology Branch, NIDDK, Bethesda, MD
- Christopher Cox, PhD, The Johns Hopkins University, Baltimore, MD
- Myles Faith, PhD, University of Pennsylvania School of Medicine, Philadelphia, PA
- I. Sadaf Farooqi, MD, Cambridge Institute for Medical Research, Cambridge, UK
- Oksana Gavrilova, PhD, Mouse Metabolism Core Laboratory, NIDDK, Bethesda, MD
- Alexander Gorbach, PhD, Laboratory of Bioengineering and Physical Science, NIBIB, Bethesda, MD
- Van S. Hubbard, MD, PhD, Division of Nutritional Research Coordination, NIDDK, Bethesda, MD
- Joel E. Kleinman, MD, PhD, Clinical Brain Disorders Branch, NIMH, Bethesda, MD
- Rudolph L. Leibel, MD, Columbia University College of Physicians and Surgeons, New York, NY
- Bronwen Martin, PhD, OSD/LCI/DS, NIA, Bethesda, MD
- Keri Martinowich, PhD, LMPET/SMCN, NIMH, Bethesda, MD
- Stephen O'Rahilly, MD, Cambridge Institute for Medical Research, Cambridge, UK
- Dale A. Schoeller, PhD, University of Wisconsin, Madison, WI
- Marian Tanofsky-Kraff, PhD, USUHS Department of Psychology, Bethesda, MD
- Lino Tessarollo, PhD, NCI Frederick Mouse Cancer Genetics Program, Frederick, MD
- George R. Uhl, MD, PhD, Molecular Neurobiology Branch, NIDA, Baltimore, MD
- B. Timothy Walsh, PhD, Columbia University College of Physicians and Surgeons, New York, NY
- Heiner Westphal, MD, Program on Genomics of Differentiation, NICHD, Bethesda, MD
- Denise E. Wilfley, PhD, Washington University School of Medicine, St. Louis, MO
- Alexander F Wilson, PhD, Inherited Disease Research Branch, NHGRI, Baltimore, MD
- Susan Z. Yanovski, MD, Obesity and Eating Disorders Program, NIDDK, Bethesda, MD
Contact
For further information, contact yanovskj@mail.nih.gov or visit ugo.nichd.nih.gov.