Mechanisms of Disease in Preterm Labor and Complications of Prematurity; Prenatal Diagnosis of Congenital Anomalies

- Roberto Romero, MD, DMedSci, Chief, Perinatology Research Branch
Preterm birth is the leading cause of perinatal morbidity and mortality worldwide. The cost of prematurity in the U.S. alone is estimated to be $26 billion per year. An important goal is to understand the mechanisms of disease responsible for spontaneous preterm birth and fetal injury and to develop methods for the prediction and prevention of preterm birth.
The Perinatology Research Branch (PRB) has proposed that preterm parturition is a syndrome caused by many pathologic processes, i.e., that preterm labor is one syndrome but has many causes. The emphasis of our Branch is to study intra-amniotic infection and inflammation, vascular disorders, maternal antifetal rejection (chronic inflammatory lesions of the placenta), cervical disease, and a decline in progesterone action. Previously, we reported that intra-amniotic inflammation, which affects at least one out of every three preterm neonates, is characterized by the activation of amniotic-fluid neutrophils, cells that represent the first line of defense against infection. Using DNA fingerprinting, we determined that amniotic-fluid neutrophils are of fetal origin in cases of preterm labor, maternal origin in cases of clinical chorioamnionitis at term, and mixed origin in patients who have inflammatory processes near term. Moreover, in a series of studies, we were able to demonstrate that neutrophils produce antimicrobial peptides and exhibit the formation of extracellular traps, whereby they immobilize and kill bacteria.
The Branch also studies other obstetrical syndromes that account for the high rate of infant mortality in the United States, including clinical chorioamnionitis, which is the most common infection-related diagnosis in delivery units around the world, as well as meconium aspiration syndrome and amniotic fluid embolism.
Congenital anomalies continue to be a leading cause of perinatal mortality in the U.S. Imaging, a powerful tool for scientific discovery, has changed the practice of obstetrics and maternal-fetal medicine. Imaging with ultrasound allows the definition of fetal anatomy, biometry, growth, and the study of physiologic parameters, such as cardiac function, fetal sleep, and breathing. We invented a new method for the examination of the fetal heart, called fetal intelligent navigation echocardiography (FINE). We recently reported a further major breakthrough: Color Doppler FINE. Color-flow mapping is essential for adequate examination of the fetal heart in those suspected of having congenital anomalies. We demonstrated how Color Doppler FINE can be used to improve the diagnosis of congenital anomalies. The technology has been licensed and is now commercially available to sonographers worldwide. We also determined the sensitivity and specificity of FINE in fetuses with normal hearts and congenital heart disease in the second and third trimesters.
Although ultrasound is the standard imaging modality in pregnancy, magnetic resonance imaging (MRI) has also been used to characterize fetal anatomy when ultrasound cannot provide definitive diagnostic answers. MRI provides unique information about fetal physiologic parameters (i.e., perfusion, oxygenation, and biochemistry) that are outside the domain of ultrasound. Moreover, MRI can be used to characterize the ontogeny of functional neuroconnectivity, as well as the potential relationship between insults that could alter fetal neurodevelopment. Given that preterm birth is a leading cause of neurodevelopmental disorders, we used noninvasive methods to interrogate neuroconnectivity. In previous work, we reported a study showing that fetuses subsequently born preterm have a disorder of neuroconnectivity not seen in fetuses of the same gestational age subsequently born at term. Neuroconnectivity was reduced in the left hemisphere, close to the prelanguage region, providing the first evidence that a disorder of functional connectivity is present in the fetus before birth.
Does the human placenta delivered at term have a microbiota?
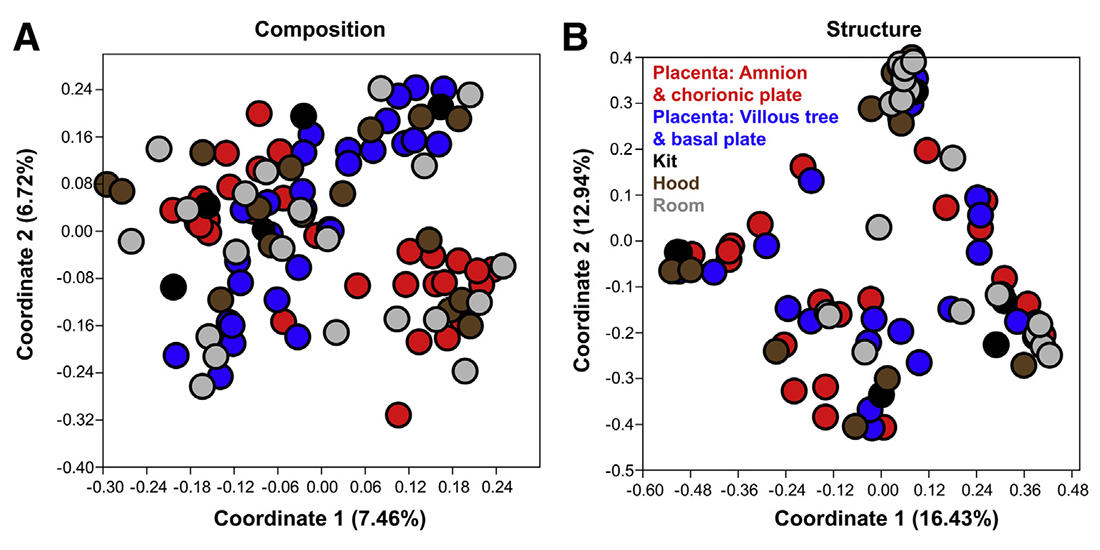
Traditionally, the human placenta has been viewed as sterile, and colonization of the placenta by microorganisms has been associated with adverse pregnancy outcomes. Yet, recent reports employing DNA sequencing techniques have reported that the human placenta at term contains a unique microbiota. However, when studying low microbial biomass samples, sequence-based approaches can capture background contaminating DNA from DNA extraction kits, PCR reagents, and laboratory environments. The objective of this study was therefore to determine whether the human placenta delivered at term in patients without labor, undergoing Cesarean delivery, harbors a resident microbiota. This was a cross-sectional study of placentas from 29 women who had a Cesarean delivery without labor at term. The study included technical controls to account for potential background contaminating DNA. The bacterial profiles of placental tissues and background technical controls were characterized and compared using bacterial culture, quantitative real-time PCR, 16S rRNA gene sequencing, and metagenomic surveys. Twenty-eight of 29 placental tissues were negative for bacterial culture. The few bacteria cultured from the remaining sample were likely laboratory contaminants because corresponding 16S rRNA genes from the cultivars were not detected in the same placental sample. Quantitative real-time PCR did not indicate greater abundances of bacterial 16S rRNA genes in placental tissues than in background technical controls. Furthermore, 16S rRNA gene sequencing did not reveal consistent differences in the composition or structure of bacterial profiles between placental samples and background technical controls (Figure 1).
Click image to view.
Figure 1. Principal coordinates analyses
The analyses illustrate similarity in 16S rRNA gene profiles among the amnion and chorionic plate, villous tree and basal plate, and technical control samples.
Most of the bacterial sequences obtained from metagenomic sequencing of placental tissues were from cyanobacteria, aquatic bacteria, or plant pathogens; the placenta is therefore unlikely to provide a suitable ecological niche for these bacteria and, as such, these data are not likely indicative of a placental microbiota. In summary, a resident microbiota could not be identified in human placentas delivered at term from women without labor, using several modes of microbiologic inquiry. A consistently significant difference in the abundance and/or presence of a microbiota between placental tissue and background technical controls could not be found. The study demonstrates that incorporating technical controls for potential sources of background contaminating DNA into studies of low microbial biomass samples, such as the placenta, is necessary in order to derive reliable conclusions about host-associated microbiota.
Antibiotics can eradicate intra-amniotic infection or inflammation.
In a case study, 50 women with singleton gestations between 20–34 weeks, preterm labor with intact membranes, and evidence of intra-amniotic infection or inflammation, by analysis of amniotic fluid obtained by abdominal amniocentesis, received an antibiotic treatment that consisted of ceftriaxone, clarithromycin, and metronidazole. Follow-up amniocentesis was performed in 19 of 29 patients who were undelivered for 7 or more days. Treatment success was defined as resolution of intra-amniotic infection/inflammation or delivery at 37 or more weeks. Resolution of intra-amniotic infection/inflammation was confirmed in 79% of patients (15/19) who had a follow-up amniocentesis. Treatment success occurred in 84% of patients (16/19) who had a follow-up amniocentesis and in 32% of patients (16/50) who received the antibiotic regimen. In conclusion, the administration of antibiotics to patients with preterm labor and intact membranes with proven intra-amniotic infection/inflammation is associated with eradication of infection and inflammation in a subset of patients.
Progesterone treatment prevents preterm labor and birth induced by effector and activated T cells.
Preterm birth is the leading cause of perinatal morbidity and mortality worldwide, which is commonly preceded by spontaneous preterm labor. Many etiologies have been associated with preterm labor; yet, only pathological inflammation has been causally linked to preterm birth. Pathological inflammation can be acute or chronic in nature. Most research has focused on the mechanisms whereby the maternal innate immune system induces acute inflammation, leading to preterm labor and birth. However, the role of the maternal adaptive immune system, specifically T cells, in the pathogenesis of preterm labor and birth was poorly understood. In the above-mentioned study, we used human tissues and animal models to investigate a causal link between maternal T cell activation and preterm labor and birth.
First, by performing exhaustive immunophenotyping of the decidual tissues, we found that effector and activated T cells are present at the human maternal-fetal interface. Importantly, the cells were enriched in women who underwent spontaneous preterm labor and birth. Next, using a murine model of in vivo T cell activation, we reported that the activation of maternal T cells induces preterm birth and adverse neonatal outcomes. The mechanisms whereby the activation of T cells induces preterm birth included stereotypical immune responses at the maternal-fetal interface as well as in the mother and the fetus, which were different from those initiated by microbial products (e.g., endotoxin) or progesterone withdrawal function (e.g., treatment with RU486). We also showed that activation of T cells induces proinflammatory responses in the myometrium and cervix. Lastly, we showed that pretreatment with progesterone, a clinically proven strategy, has systemic and local anti-inflammatory effects preventing preterm birth and adverse neonatal outcomes. Collectively, the findings reported in this study provide the first mechanistic demonstration of a role for maternal effector and activated T cells in the pathophysiology of preterm labor and birth (Figure 2).

Click image to view.
Figure 2. Conceptual framework
Effector and activated T cells expressing granzyme B and perforin can induce pathologic inflammation by initiating local immune responses at the maternal-fetal interface (decidua) (i.e., activation of B cells and an M1-like macrophage polarization without an increased influx of neutrophils), which, in turns, leads to preterm labor and birth. Activation of T cells also induces inflammatory responses in the maternal circulation and the amniotic cavity, inducing fetal damage prior to preterm labor and birth. These effects can be abrogated by treatment with progesterone, a clinically approved strategy.
Fetal biometry as a predictor of adverse perinatal outcomes
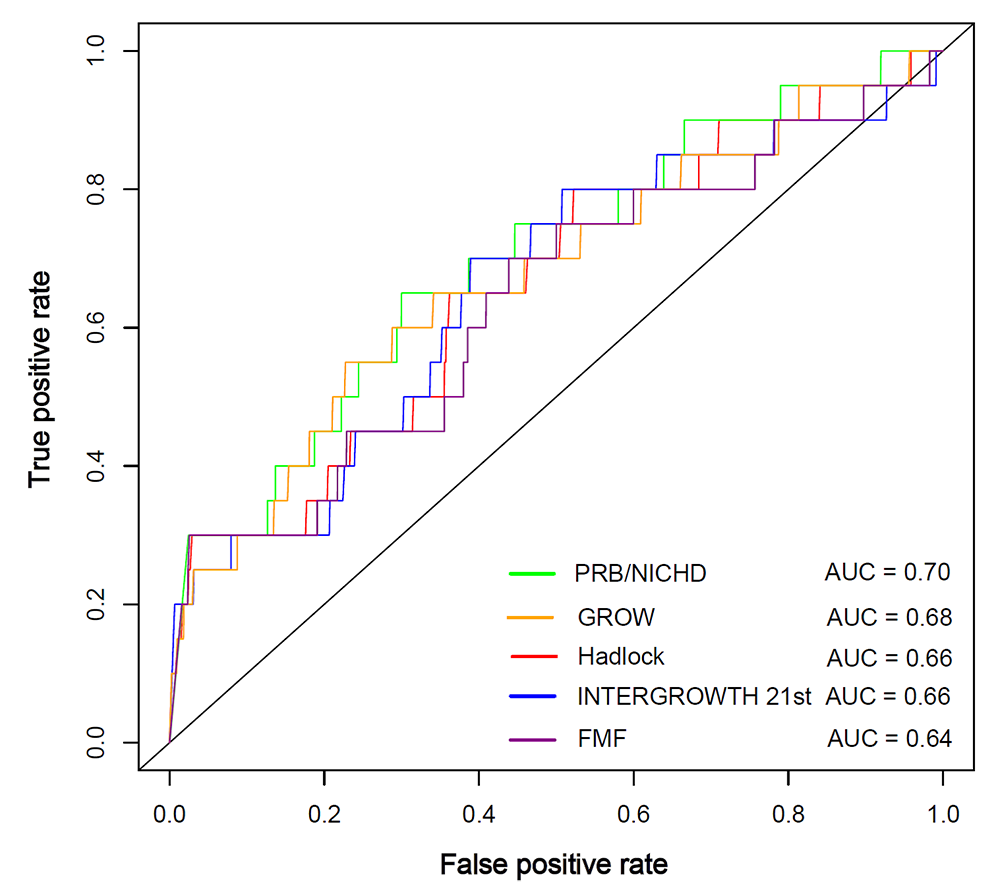
A basic need in prenatal care is an evaluation of adequacy of fetal growth. Although many fetal growth standards have been proposed, there is no consensus on the best standard to use in practice. We therefore compared the predictive ability of estimated fetal weight (EFW) percentiles, according to seven growth standards, to detect fetuses at risk for adverse perinatal outcomes in a retrospective cohort of 3,437 African-American women. The standards are as follows: the one-fits-all (Hadlock, INTERGROWTH-21st, WHO, FMF), ethnic-specific (NICHD), fetal sex and maternal characteristics–customized (GROW), and African-American–customized (PRB/NICHD) growth standards were applied to the last available scan prior to delivery. We found, among others, that fetuses with an EFW at or below the 10th percentile as well as those with an EFW at or above 90th percentile were at increased risk for adverse perinatal outcomes according to all, or some, of the seven standards, respectively. The relative risk carried by an EFW at or below the 10th percentile for the composite adverse perinatal outcome was higher for the most stringent standard (NICHD) compared with the least stringent standard (FMF) in small-for-gestational-age screening. The complementary analysis based on the ROC curve analysis suggests a slightly improved detection of adverse perinatal outcomes by more recent population-based (INTERGROWTH-21st) and customized (PRB/NICHD) standards compared with the Hadlock and FMF standards (Figure 3).
Click image to view.
Figure 3. Receiver Operating Characteristic (ROC) curves for the prediction of perinatal death
The ROC curves are constructed from the percentile of estimated fetal weight according to each standard, and the area under the curves (AUC) is shown in the legend. GROW: Gestational-age Related Optimal Weight; FMF: Fetal Medicine Foundation; PRB: Perinatology Research Branch.
QUEST MRI to detect oxidative stress in the fetal brain
Intra-amniotic inflammation has been implicated as a major risk for fetal brain injury, which is only diagnosable in postmortem excised tissue. In vivo and ex vivo studies have shown that fetal brain injury can be induced by oxidative stress. Therefore, the early detection of fetal brain oxidative stress may be useful to diagnose fetal injury and to provide personalized antioxidant treatment. In the above-mentioned study, we reengineered the QUEnch-assiSTed (QUEST) MRI method to measure excessive free radical production in the fetal brain. First, we created 3D printed clip to gently secure individual fetuses in situ to stabilize spontaneous breathing movements. Second, we determined the best MRI sequence (R1 data) to obtain signals without artifacts. Third, we used surface coil reception to maximize the filling factor, which resulted in improvement of the signal-to-noise ratio over a whole-body coil. Lastly, the MRI data (R1 data) were normalized to reduce coil inhomogeneities and slice bias for a more precise R1 estimate. This reengineered method was then tested in an animal model in which an ultrasound-guided intra-amniotic injection of endotoxin induced preterm birth, a pregnancy complication that is prevented by treatment with the antioxidant rosiglitazone. We report that the QUEST MRI method is capable of detecting oxidative stress in the fetal brain (green-yellow signal), which is reduced by treatment with the antioxidant rosiglitazone. The study represents the first demonstration that oxidative stress can be determined in the fetal brain using QUEST MRI.
Oxygenation and perfusion to evaluate cerebral hemodynamics in growth-restricted fetuses
We estimated venous blood oxygenation (SvO2) of the fetal brain’s superior sagittal sinus by susceptibility weighted imaging and measured the blood perfusion by power Doppler ultrasound and fractional moving blood volume from the frontal lobe in a midsagittal plane of the fetal brain. The experiments were performed on 33 healthy fetuses and 10 abnormal fetuses with fetal growth restriction. We found that SvO2 values and the trend across gestations were similar in fetal growth–restricted and healthy fetuses, while in healthy fetuses fractional moving blood volume values were higher and the trend across gestations was the opposite. We also found that, in fetal growth–restricted fetuses, the SvO2 and fractional moving blood volume association was significantly positive. Such a dual-imaging modality approach could be beneficial for early detection of fetal brain sparing and brain oxygenation saturation changes in high-risk pregnancies.
Publications
- Theis KR, Romero R, Winters AD, Greenberg JM, Gomez-Lopez N, Alhousseini A, Bieda J, Maymon E, Pacora P, Fettweis JM, Buck GA, Jefferson KK, Strauss III JF, Erez O, Hassan SS. Does the human placenta delivered at term have a microbiota? Results of cultivation, quantitative real-time PCR, 16S rRNA gene sequencing, and metagenomics. Am J Obstet Gynecol 2019;220:267.e1-39.
- Yoon BH, Romero R, Park JY, Oh KJ, Lee J, Conde-Agudelo A, Hong JS. Antibiotic administration can eradicate intra-amniotic infection or intra-amniotic inflammation in a subset of patients with preterm labor and intact membranes. Am J Obstet Gynecol 2019;221(2):142.e1-142.e22.
- Arenas-Hernandez M, Romero R, Xu Y, Panaitescu B, Garcia-Flores V, Miller D, Ahn H, Done B, Hassan SS, Hsu CD, Tarca AL, Sanchez-Torres C, Gomez-Lopez N. Effector and activated T cells induce preterm labor and birth that is prevented by treatment with progesterone. J Immunol 2019;202(9):2585-2608.
- Kabiri D, Romero R, Gudicha DW, Hernandez-Andrade E, Pacora P, Benshalom-Tirosh N, Tirosh D, Yeo L, Erez O, Hassan SS, Tarca AL. Prediction of adverse perinatal outcomes by fetal biometry: a comparison of customized and population-based standards. Ultrasound Obstet Gynecol 2020;55(2):177-188.
- Yadav B, Hernandez-Andrade E, Krishnamurthy U, Buch S, Jella P, Trifan A, Yeo L, Hassan SS, Haacke EM, Romero R. Dual-imaging modality approach to evaluate cerebral hemodynamics in growth-restricted fetuses: oxygenation and perfusion. Fetal Diagn Ther 2020;47(2):145-155.
Collaborators
- Tinnakorn Chaiworapongsa, MD, Wayne State University School of Medicine, Detroit, MI
- Agustin Conde-Agudelo, MD, Wayne State University School of Medicine, Detroit, MI
- Mark Haacke, PhD, Wayne State University School of Medicine, Detroit, MI
- Leonid Margolis, PhD, Section on Intercellular Interactions, NICHD, Bethesda, MD
- Adi L. Tarca, PhD, Wayne State University, Detroit Medical Center, Detroit, MI
- Lami Yeo, MD, Wayne State University School of Medicine, Detroit, MI
- Bo Hyun Yoon, MD, PhD, Seoul National University, Seoul, Korea
Contact
For more information, email romeror@mail.nih.gov or visit http://irp.nih.gov/pi/roberto-romero.


