Mechanisms of Disease in Preterm Labor and Complications of Prematurity; Prenatal Diagnosis of Congenital Anomalies

- Roberto Romero, MD, DMedSci, Chief, Program in Perinatal Research and Obstetrics
Preterm birth is the leading cause of perinatal morbidity and mortality worldwide. The cost of prematurity in the U.S. alone is estimated to be $26 billion per year. An important goal is to understand the mechanisms of disease responsible for spontaneous preterm birth and fetal injury and to develop methods for the prediction and prevention of preterm birth.
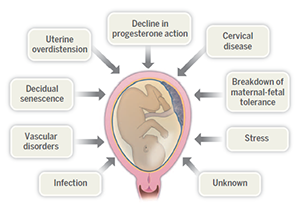
The Perinatology Research Branch (PRB) has proposed that preterm parturition is a syndrome caused by multiple pathologic processes (Preterm labor: one syndrome, many causes. Science 2014;345:760; also Figure 1). The emphasis of our Branch has been to study intra-amniotic infection and inflammation, vascular disorders, maternal anti-fetal rejection (chronic inflammatory lesions of the placenta), cervical disease, and a decline in progesterone action. This year, we report that point-of-care tests can be employed for the rapid diagnosis of intra-amniotic inflammation (within 20 minutes) and also evidence that a new combination of antimicrobial agents can reduce the risk of adverse pregnancy outcome and histologic inflammation. Given that one third of all preterm deliveries are the result of physician-initiated birth owing to preeclampsia or intrauterine growth restriction, we also studied the role of biomarkers in the prediction of indicated preterm delivery in mothers carrying small-for-gestational age fetuses. We report for the first time biomarkers for the presence of placental histologic lesions consistent with maternal vascular under-perfusion. The lesions underlie most cases of fetal death, preeclampsia, severe and early fetal growth restriction, and a fraction of spontaneous preterm labor.
Click image to enlarge.
Figure 1. Proposed mechanisms of disease responsible for the preterm parturition syndrome
From: Romero R, Dey SK, Fisher SK. Preterm labor: one syndrome, many causes. Science 2014;345(6198):760.
The Branch also studies other obstetrical syndromes that account for the high rate of infant mortality in the United States, including clinical chorioamnionitis, which is the most common infection-related diagnosis in delivery units around the world, as well as meconium aspiration syndrome and amniotic fluid embolism.
Congenital anomalies continue to be a leading cause of perinatal mortality in the United States. A powerful tool for scientific discovery, imaging has changed the practice of obstetrics and maternal-fetal medicine. Imaging with ultrasound allows the definition of fetal anatomy, biometry, growth, and the study of physiologic parameters, such as cardiac function, fetal sleep, and breathing. Our studies with three-dimensional and four-dimensional ultrasound continue as does the clinical testing of fetal intelligent navigation echocardiography (FINE), a technology invented by our Branch and licensed and commercially available.
Although ultrasound is the standard imaging modality in pregnancy, magnetic resonance imaging (MRI) has also been used to characterize fetal anatomy when ultrasound cannot provide definitive diagnostic answers. MRI provides unique information about fetal physiologic parameters (i.e., perfusion, oxygenation, and biochemistry) that are outside the domain of ultrasound. Moreover, MRI can be used to characterize the ontogeny of functional neuroconnectivity, as well as the potential relationship between insults which could alter fetal neurodevelopment. We therefore developed methods to use quantitative MRI to gain insight into the fetal brain anatomy and physiology.
Progesterone for the prevention of preterm birth in women with a short cervix
We previously reported the results of the PREGNANT trial and an individual patient meta-analysis, as well as a cost-effective analysis, indicating that vaginal progesterone given to patients with a short cervix reduces the rate of preterm birth (less than 33 weeks of gestation) by 45%, admission to the NICU, respiratory distress syndrome, requirement for mechanical ventilation, and neonatal morbidity. This has led to a change in practice, as professional organizations (American Congress of Obstetricians and Gynecologists, Society for Maternal-Fetal Medicine) have recommended treatment with vaginal progesterone to patients with a short cervix. The International Federation of Gynecology and Obstetrics (FIGO) has endorsed universal cervical screening to identify patients at risk for preterm delivery and the administration of vaginal progesterone to prevent preterm birth.
In February 2016, investigators in the U.K. reported results of the OPPTIMUM trial (a multi-center, randomized, double-blind trial of vaginal progesterone prophylaxis for preterm birth). This trial enrolled (1) 903 patients with a prior history of previous spontaneous preterm birth at less than 34 weeks; (2) 251 patients with a short cervix (less than 25mm); and (3) patients with a positive fetal fibronectin test combined with other clinical risk factors for preterm birth. Overall, the investigators reported that vaginal progesterone did not reduce the rate of preterm birth. However, we (and others) believe that this was attributable to important limitations in study design, as well as inadequate sample size and compliance. Indeed, there was a non-significant trend towards a reduction in preterm delivery in patients with a cervical length of less than 25mm.
We contacted the authors to perform an individual patient meta-analysis and, in the meantime, performed a systematic review and aggregate meta-analysis. We uncovered that the OPPTIMUM trial was at high risk for attrition, reporting, and compliance biases.
Importantly, we found that after adding the results of the OPPTIMUM trial to our previous individual patient data meta-analysis, vaginal progesterone significantly reduced the rate of preterm birth. We are expecting delivery of the data from the OPPTIMUM investigators to conduct an individual patient meta-analysis (as agreed upon with Dr. Jane Norman at the Royal College of Obstetricians and Gynecologists meeting in October, 2016).
Vaginal progesterone, but not 17-alpha-hydroxyprogesterone caproate, has anti-inflammatory effects.
As stated above, the main strategy for the prevention of preterm birth is the administration of progestogens. Vaginal progesterone, a natural steroid hormone, is offered to women with a short cervix as it reduces the rate of preterm birth by 45% and neonatal morbidity. The other progestogen is 17-alpha-hydroxyprogesterone caproate (17-OHPC), a synthetic progestin, offered to women with a history of preterm birth.
The mechanisms whereby progestogens prevent preterm birth are unknown. We explored whether the beneficial effect of progestogens can be attributed to immunomodulation. We found that vaginal progesterone (but not 17OHP-C) (1) reduced the number of neutrophils and monocytes expressing matrix-metalloproteinase 9 (MMP-9) in the uterine cervix; (2) reduced the number of decidual macrophages and myometrial neutrophils expressing IFNγ; (3) raised the number of regulatory T cells in the decidua; and (4) prevented endotoxin-induced preterm birth. The results explain the difference in efficacy of vaginal progesterone vs. 17OHP-C in the prevention of preterm birth in patients with a short cervix. The study provides insight into the mechanisms whereby vaginal progesterone prevents preterm birth in women with a sonographic short cervix.
The inflammasome in spontaneous labor at term
Transcriptomic studies have indicated that spontaneous parturition at term is characterized by an inflammatory signature. The first cytokine to be implicated in the mechanisms of normal parturition was interleukin-1β (IL-1β), and it is now well established that this cytokine plays a central role both in term and preterm labor. However, spontaneous parturition at term represents an example of sterile inflammation, not microbial-induced inflammation. Therefore, a fundamental question is how IL-1β is activated in spontaneous labor at term.
We reported several studies showing that the inflammasome, a cytosolic signaling platform, participates in the activation of caspase-1 which, in turn, promotes the processing of mature IL-1β in the chorioamniotic membranes from women who had undergone spontaneous labor at term. These observations are consistent with our previous reports that caspase-1 is overexpressed in women with spontaneous labor at term, as well as in those with preterm labor. This is the first demonstration that inflammasome complexes are involved in physiologic parturition.
Intra-amniotic administration of the alarmin HMGB1 induces spontaneous preterm labor and delivery.
Sterile intra-amniotic inflammation is frequently present in patients with preterm labor and intact membranes, prelabor rupture of membranes, a sonographic short cervix, and cervical insufficiency. The mechanisms responsible for sterile intra-amniotic inflammation–induced preterm delivery have not been elucidated. We proposed that alarmins released during the process of cellular stress or cell death can induce spontaneous preterm parturition. In support of this, we found that the prototypic alarmin high-mobility group box-a (HMGB1) is present in high concentrations in women with preterm labor and sterile intra-amniotic inflammation.
To determine whether an elevated amniotic fluid concentration of HMGB1 can induce preterm labor, we administered HMGB1 intra-amniotically to pregnant mice under ultrasound guidance and found that this alarmin can induce preterm labor and delivery. This is the first evidence that an alarmin can induce preterm parturition. The observations are important because a substantial number of patients with intra-amniotic inflammation do not have microbial invasion of the amniotic cavity, which can be demonstrated using cultivation and molecular microbiologic techniques. The results identify novel mechanisms of disease for preterm labor, raise questions about the mechanisms whereby alarmins can induce preterm labor, and identify potential therapeutic targets.
Fetal intelligent navigation echocardiography (FINE)
Congenital heart disease is the leading cause of neonatal death for congenital anomalies, and the current sensitivity for the prenatal diagnosis of congenital heart disease (CHD) is the lowest. We invented a method for the visualization of standard echocardiography views from volume datasets (fetal intelligent navigation echocardiography or FINE), which is based on obtaining dataset volumes with spatio-temporal image correlation (STIC). This invention was first published in 2013 and licensed to an ultrasound company and is commercially available worldwide.
The standard obstetrical practice is to perform fetal echocardiography with 2-dimensional ultrasound. The use of FINE requires the acquisition of cardiac datasets with 4-dimensional ultrasound. Clinical application of FINE depends upon the acquisition of informative volumes and training/education of the users. We conducted two prospective studies to determine the frequency with which STIC volumes can be acquired in the second and third trimesters of pregnancy and the frequency with which the diagnostic planes recommended by professional societies (American Institute of Ultrasound in Medicine, International Society of Ultrasound in Obstetrics and Gynecology) can be obtained. In the first study, one or more STIC volumes were successfully obtained in 72.5% (150/207) of patients, of which 96.2% were considered “informative.” The nine diagnostic planes were obtained in 76–100% of cases using only the “Diagnostic Plane” feature, and 98–100% when the “Virtual Intelligent Sonographer Assistance” (VIS-Assistance) was employed. Given that FINE was invented at the PRB, we conducted a separate prospective study in a collaborative center in Italy with physicians not involved in the development of FINE, but who were trained in this method at the PRB. One or more STIC volumes were captured from 246 patients, and the diagnostic planes could be obtained in 96–100% of cases in the second and third trimesters. Collectively, these observations indicate that FINE can be used as a method of screening for CHD and is easily exported to the clinical setting.
This year, we developed a method to perform FINE using color STIC (or color FINE), an addition that is essential for the evaluation of the fetus at risk for CHD and which allows refinement in the diagnosis of abnormal fetal hearts. We have already used color FINE to improve the diagnosis of complex disorders (e.g., hypoplastic left heart, coarctation of the aorta, heterotaxia with interrupted inferior vena cava, etc.).
Publications
- Romero R, Nicolaides KH, Conde-Agudelo A, O'Brien JM, Cetingoz E, Da Fonseca E, Creasy GW, Hassan SS. Vaginal progesterone decreases preterm birth =34 weeks of gestation in women with a singleton pregnancy and a short cervix: an updated meta-analysis including data from the OPPTIMUM study. Ultrasound Obstet Gynecol 2016;48:308-317.
- Furcron AE, Romero R, Mial TN, Balancio A, Panaitescu B, Hassan SS, Sahi A, Nord C, Gomez-Lopez N. Human chorionic gonadotropin has anti-inflammatory effects at the maternal-fetal interface and prevents endotoxin-induced preterm birth, but causes dystocia and fetal compromise in mice. Biol Reprod 2016;94:136.
- Gomez-Lopez N, Romero R, Plazyo O, Panaitescu B, Furcron AE, Miller D, Roumayah T, Flom E, Hassan SS. Intra-amniotic administration of HMGB1 induces spontaneous preterm labor and birth. Am J Reprod Immunol 2016;75:3-7.
- Romero R, Xu Y, Plazyo O, Chaemsaithong P, Chaiworapongsa T, Unkel R, Than NG, Chiang PJ, Dong Z, Xu Z, Tarca AL, Abrahams VM, Hassan SS, Yeo L, Gomez-Lopez N. A role for the inflammasome in spontaneous labor at term. Am J Reprod Immunol 2016;Epub ahead of print.
- Garcia M, Yeo L, Romero R, Haggerty D, Giardina I, Hassan SS, Chaiworapongsa T, Hernandez-Andrade E. Prospective evaluation of the fetal heart using Fetal Intelligent Navigation Echocardiography (FINE). Ultrasound Obstet Gynecol 2016;47:450-459.
Collaborators
- Tinnakorn Chaiworapongsa, MD, Wayne State University School of Medicine, Detroit, MI
- Agustin Conde-Agudelo, MD, Wayne State University School of Medicine, Detroit, MI
- Jean-Charles Grivel, PhD, Section on Intercellular Interactions, NICHD, Bethesda, MD
- Mark Haacke, PhD, Wayne State University School of Medicine, Detroit, MI
- Sonia Hassan, MD, Wayne State University School of Medicine, Detroit, MI
- Edgar Hernandez-Andrade, MD, Wayne State University School of Medicine, Detroit, MI
- Dan Dongeun Huh, PhD, University of Pennsylvania, Philadelphia, PA
- Chong-Jai Kim, MD, University of Ulsan College of Medicine, Asan Medical Center, Seoul, Korea
- Steven J. Korzeniewski, PhD, MSc, MA, Wayne State University School of Medicine, Detroit, MI
- Leonid Margolis, PhD, Section on Intercellular Interactions, NICHD, Bethesda, MD
- Adi L. Tarca, PhD, Wayne State University, Detroit Medical Center, Detroit, MI
- Moriah Thomason, PhD, Wayne State University School of Medicine, Detroit, MI
- Lami Yeo, MD, Wayne State University School of Medicine, Detroit, MI
- Bo Hyun Yoon, MD, PhD, Seoul National University, Seoul, Korea
Contact
For more information, email romeror@mail.nih.gov or visit irp.nih.gov/pi/roberto-romero.


